Bed sores, sometimes referred to as pressure ulcers or decubitus ulcers in medicine, are painful wounds that commonly affect those with limited movement. These ulcers form as a result of sustained pressure applied to the skin and underlying tissues, typically on weight-bearing body parts including the hips, elbows, and heels. Bed sores continue to be a problem in hospital settings despite being generally preventable, creating difficult situations for both patients and healthcare professionals. Understanding the root reasons for bed sore development is vital for finding effective solutions to this problem.
In this article, we examine the many different aspects that lead to the development of bed sores. We examine the interrelated network of causes, including everything from the harmful effects of prolonged immobility and decreased blood circulation to the involvement of friction, shear pressures, and poor nutrition. By identifying these factors, we hope to provide readers with useful information about bed sore management and prevention, thereby enhancing the well-being and standard of life for those who are at risk. Join us as we solve the puzzle of bed sores and equip patients and caregivers with the knowledge they need to confront this common and treatable ailment like how can creams help with bed sores.
Causes of Bedsores
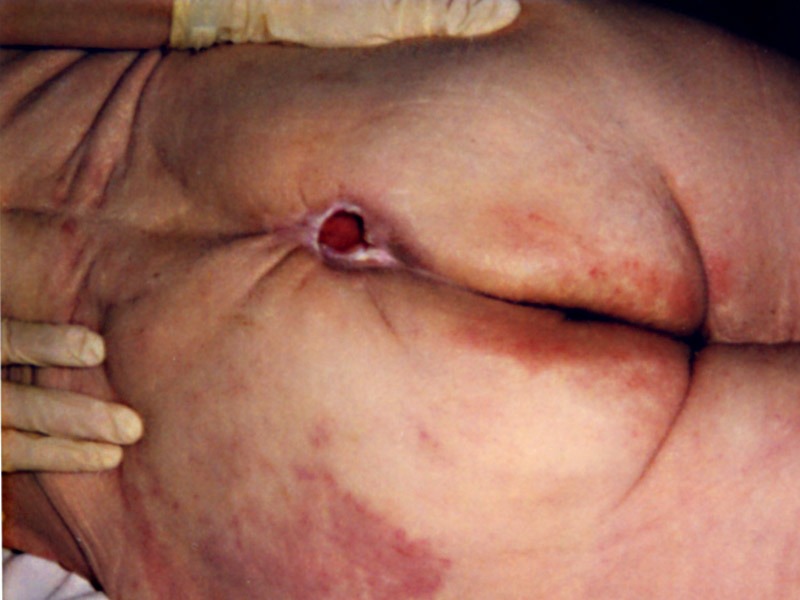
When the skin’s blood flow is interrupted for longer than two to three hours, a bedsore forms. The bedsore begins as a red, painful patch that eventually turns purple as the skin dies. If the skin is not treated, it may crack open, allowing an infection to spread.
Deep bedsores might develop. It may penetrate bone and muscle. A bedsore usually heals quite slowly once it starts to form. Bedsores can take days, months, or even years to heal, depending on their severity, the patient’s health, and the existence of underlying conditions (such diabetes). To speed up the healing process, they could require surgery.
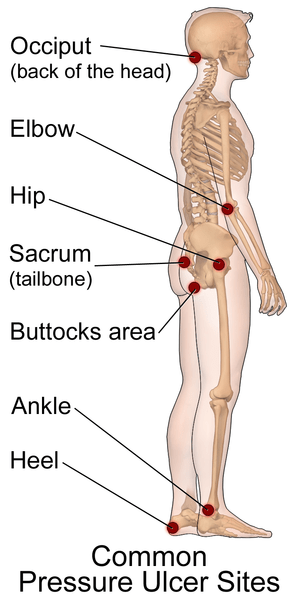
Bedsores frequently develop on the:
- Buttocks area (on the tailbone or hips)
- Heels of the feet
- Shoulder blades
- Back of the head
- Back and sides of the knees
Other Names for Bedsores
- Decubitus ulcers.
- Pressure injuries.
- Pressure sores.
- Pressure ulcers.
- Pressure wounds.
What Are The Risk For Bedsores?
A bedsore is more likely to form if a person is immobilized, unconscious, bedridden, or unable to feel pain. If the person is not turned, positioned correctly, or given access to proper diet and skin care, the risk rises. Malnutrition, circulation issues, and diabetes all increase risk.
Stages of Bedsores
From least severe to most severe, bedsores are categorized into 4 phases. Which are:
- Stage 1 – The region is heated to the touch and appears red. The area could seem blue or purple on people with darker complexion. Additionally, the person may claim that it stings, aches, or itches.
- Stage 2 – There may be an open sore, scrape, or blister in the area, which appears to be more damaged. Significant pain is reported by the patient, and the skin near the lesion may appear discolored.
- Stage 3 – The injury beneath the skin’s surface gives the area a crater-like look.
- Stage 4 – The area is severely damaged, and there is a big wound. It can affect the bones, joints, muscles, and tendons. Infection is currently a significant concern.
When there is full-thickness tissue loss and peel or irritation is present in the wound bed, the ulcer’s base is not given a stage. It can be brown, yellow, green, grey, or tan in color. Eschar typically has a tan, brown, or black color.
How Common are Bedsores?
According to experts, 2.5 million Americans get bedsores each year. Bedsores can affect anyone.
What are the Complication of Bedsores?
Your risk of potentially fatal bacterial infections like cellulitis and septicemia is increased by bed sores. You can become septic or need to have an amputation. Each year, more than 24,000 deaths due to bedsores occur in the world.
Some persons experience the development of sinus tracts, which are openings that link the deeper bodily tissues affected by the pressure sore damage. You could develop depending on how the sinus tract is connected.
- Bacteremia, or the presence of bacteria in the blood, can cause bacterial endocarditis or meningitis.
- Osteomyelitis or septic arthritis are infections of the bones or joints, respectively.
- Infections caused by Group A streptococcus, ranging from cellulitis to necrotizing fasciitis (a condition that consumes flesh).
How are Bedsores Diagnosed
For diagnosis and treatment, you might visit a wound specialist. Bed sores are classified and staged by medical professionals based on their appearance. To track how the wound is healing, your doctor will take a picture of the sore.
To screen for infections, you might undergo certain tests, such as:
- Biopsies.
- Blood tests and cultures.
- MRIs or X-rays.
Nonsurgical Treatment for Bedsores
Stages 1 or 2 bedsores may be treated by you or a carer. You might visit a wound specialist for bedsores that are in stages 3 or 4. The amount of time it takes for the sore to heal will depend on how severe the pressure ulcer was.
You or your healthcare professional may do the following to treat a pressure injury:
- Saline (a sterile saltwater solution) or soap and water should be used to clean or irrigate the wound.
- Use specific medical bandages intended to encourage healing to dress (cover) the wound. These include foam dressings, alginates (seaweed), hydrocolloid, and water-based gel (hydrogel).
Your healthcare professional will perform a process known as debridement to remove dead tissue from deep, severe pressure ulcers. A tool called a scalpel is used by your provider to remove the dead tissue. The dead tissue can also be removed from your body by using ointments that they may apply. Even if the tissue is dead, the area around it isn’t, so your healthcare professional might use a local anesthetic to numb the area first.
Treatment and Prevention
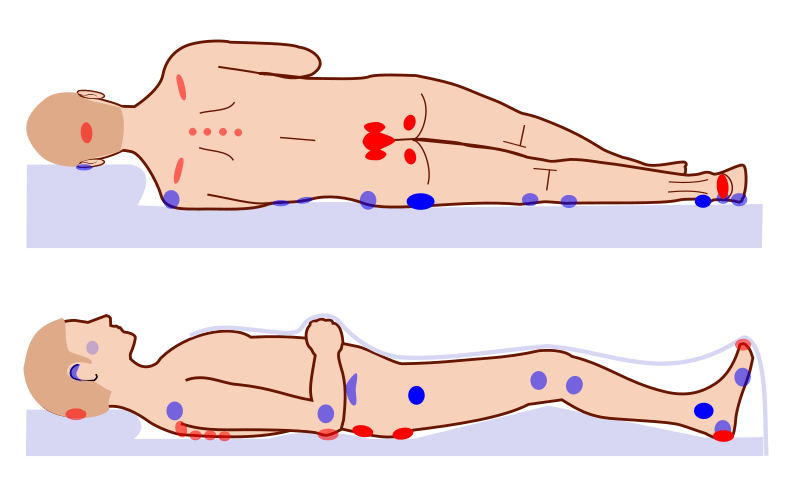
Moving about frequently is the greatest way to avoid bedsores.
This will prevent pressure from building up on your body, distribute your weight more evenly, and encourage blood flow to the tissues. If you are unable to move, you should be assisted to change positions at least every two hours in bed or every fifteen minutes in a chair. If you are unable to move, pillows or foam wedges can assist in shifting your weight. Exercises that increase range of motion can enhance circulation, maintain muscular mass, and assist prevent contractures.
To lessen shearing pressures, your bed shouldn’t be elevated by more than 30 degrees (except from when you’re eating). A pull-sheet should be used to assist with changing positions in bed for the same purpose.
Some people find a convoluted “egg-crate” foam pad to be a cheap and portable alternative
This sturdy, 5 to 10 cm high-density foam pad is less likely to be squeezed by your weight and could efficiently redistribute your weight. Unfortunately, these pads only somewhat relieve pressure and may induce a buildup of body heat, which heightens perspiration. If your activity is time-limited, they can be helpful. Alternating between pressure and water mattresses could be beneficial.
Even if sheepskin isn’t thick or dense enough to relieve pressure, some people find it helpful if they are prone to skin abrasion from friction. For instance, if you have vascular problems, a sheepskin at the foot of your bed may reduce friction against your heels.
Splints can be utilized as well, and they should be applied to pressure points
Additionally, specially designed anatomically shaped cushions aid in appropriately dispersing your weight and preventing pressure points from developing. Pads with specific shapes may be needed for the elbows and heels. Some medical supply businesses provide bed cradles that lift the weight of your covers off of your body and construct a device similar to a tent.
You ought to frequently examine and clean your skin
It might become infected and develop sores if it isn’t kept dry and clean. Applying as little force and friction as possible, the affected area should be gently cleaned with plain water or a tiny amount of mild soap and water. The natural oils that protect the skin are removed by soap, and the cleansing activity may irritate tissues that are already injured. Next, a little layer of moisturizing lotion should be applied, gently massaging the reddish area or bony prominence around it rather than over it. A strong massage may worsen tissue damage by creating shearing forces. After moisturizing the area, apply a thin coating of a petroleum-based product. These water-repellent products provide a barrier of protection. Although protective, heavy chemicals like zinc oxide and aluminum paste shouldn’t be used since they are difficult to remove.
Use caution while using condom catheters, indwelling bladder catheters, or absorbent incontinence briefs. Despite being useful, these devices shouldn’t be used in place of programs to help people manage their bowel and bladder functions in order to help them restore continence.
Bed sores should be treated by a nurse or physician
Since recovery may take some time, prevention is the best course of action.
The severity (i.e., stage) of the skin wound determines how bedsores should be treated
Various methods may be employed to encourage healing depending on the severity. They include acetic acid compresses, hydrocolloid dressings, synthetic dressings, saline dressings, radiant heat dressings, and different antibiotic dressings (bedsores are particularly vulnerable to infection). Skin transplant surgery may be required to remove and replace sections of dead skin from more serious wounds. Repositioning frequently to relieve pressure is the most crucial step in treating and avoiding bedsores. In addition to treating and preventing infections, treatment also includes managing pain.
A diet high in protein may promote faster healing of wounds.
Adding protein supplements to a balanced diet may improve your chances of making a full recovery because your body requires the right nutrition to repair.
Conclusion
Understanding the causes of bed sores is essential to preventing and properly treating this painful ailment. Bed sores are largely caused by prolonged pressure, decreased blood flow, friction, shear forces, and poor nourishment. The occurrence of bed sores can be considerably decreased by addressing these causes and putting preventive measures into place, such as routine repositioning, healthy diet, and upholding good hygiene.